What To Know About Medical 3D Printing
access_timeJuly 13, 2021
By: Bryan Smith, Compliance Team Associate
- 3D printing was born in France – 3D printing, invented in France in 1984, emerged in the 21st century as a commercial technology with a variety of biocompatible materials available to medical device manufacturers.
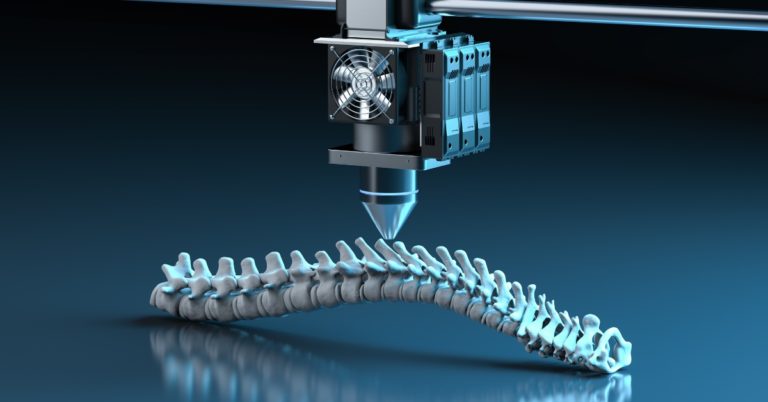
- 3D printing comes in a variety of flavors – The FDA refers to 3D printing as additive manufacturing (AM). Powder bed fusion, stereolithography, fused filament fabrication, and liquid-based extrusion are the AM technologies commonly used in medical devices.
- 3D printing is not for everyone – Determine if 3D printing is right for a product through a technical and financial feasibility assessment. First, determine if the technology meets structural and dimensional tolerance requirements. Second, perform a cost analysis against traditional manufacturing technologies such as injection molding. For low-volume custom-scaled devices, 3D printing may be a great fit, provided that dimensional tolerances can be met during printing and/or post-printing processing.
- 3D printing can create a perfect fit – 3D printing is especially useful in creating patient-specific customized devices. Patient-specific start with a full-sized template that is scaled to fit the specific geometry of a patient. Although sometimes referred to as “customized” devices, these devices do not fall under the FD&C custom device exemption requirements unless they comply with all criteria of section 520(b).
- 3D printed devices take the same regulatory pathway – The FDA anticipates that AM devices follow the same regulatory requirements, classification and submission requirements as a predicate non-AM device. In rare cases, AM may raise additional concerns over safety and/or effectiveness.
- 3D printing machines are unique – The performance of 3D printed medical devices is closely linked to control of materials, machine, and post-printing processes. 3D printers and post-post printing processes must undergo process validation to comply with the Quality System Regulation (QSR) 21CFR820. This includes IQ, OQ, and PQ. Because each printer performance is unique, even comparing machines of the same make and model, process validation must be specific to each 3D printing machine.
- 3D printing software workflow must also be validated – Several sources offer software packages that convert medical imaging files so they can be imported into 3D design and printing software. The software workflow, including the software and conversion process used in 3D printing, must also be validated.
- 3D printable biomedical models are free – The goal of the project is to facilitate the application of 3D printing in the biosciences.
- 3D printed cranial implant cleared in 2013 – In 2013, for the first time, the FDA granted 510(k) clearance for a 3D-printed polymer implant. The patient-specific cranial implant, manufactured by Oxford Performance Materials (OPM), was a spinoff from its polymer resin business, where they had traditionally supplied a special polymer raw material known as PEKK. In 2006 they began experimenting with 3D printing, and in 2011 OPM commenced biomedical additive manufacturing. Since the initial 510(k) in 2013, OPM received clearance for additional patient-specific implantable devices.
- 3D-printed bone replacement authorized in 2021 – In 2021, the FDA granted clearance of the first 3D-printed bone replacement under its humanitarian device exemption (HDE) process. The patient-specific talus spacer provides an alternative to fusion or amputation in cases of late-stage avascular necrosis (AVN) of the ankle. Under the HDE the manufacturer’s profits are restricted, as the regulatory criteria are less stringent. Premarket Authorizations (PMAs) require demonstrated effectiveness and reasonable assurance of safety, while HDEs only require probable benefit and assurance that patients will not be exposed to unreasonable/significant risk of illness or injury.
- 3D printed drugs and human tissue – Drug and human tissue products, manufactured in conjunction with 3D printing, are presently under development. While devices are regulated by the Center for Devices and Radiological Health (CDRH), drugs and human tissue are regulated by the Center for Drug Evaluation and Research (CDER) and Center for Biologics Evaluation and Research (CBER), respectively.
- 3D printed device guidance from FDA – In December 2017, the FDA issued a guidance for 3D printed medical devices: Technical Considerations for Additive Manufactured Medical Devices Guidance for Industry and Food and Drug Administration Staff Document. This was issued as a leapfrog guidance that serves as a mechanism by which the Agency shared initial thoughts regarding emerging technologies that are likely to be of public health importance early in product development.